Medical Care Testing and Treatment Options for Survivors
Survivors can access a range of healthcare services after a sexual assault including:
- Assessment and treatment of physical injuries
- Testing and preventative treatment for Sexually Transmitted Infections (STIs) and pregnancy
- Mental health support
Survivors have the right to their choice of medical services and can change their mind at any time.
During the medical assessment, a healthcare provider will ask the survivor about their medical history which can include questions about:
- Current medications
- Allergies
- Immunizations
- Sexual health history (e.g., last menstrual period)
- Pregnancy
- The sexual assault
The healthcare provider may conduct a physical exam to check for injuries with the survivor’s consent (Leduc-Robert et al., 2020; BC Women’s Hospital + Health Centre, 2017). The genital and anal area may be checked if the survivor has health concerns and consents to an exam.
Access the links below to get more information about how and when survivors can get tested and/or treatment for different injuries and conditions.
Sexual Assault and Strangulation
Concussion
Survivors should get medical care if there’s a possibility that they have a concussion from being assaulted.
Pregnancy
A urine pregnancy test is recommended between 10 days to four weeks after the sexual assault. Taking a pregnancy test too early, such as before you expect your period, can give a false negative result i.e., indicate that you are not pregnant when you are (Sexual Assault Service, BC Women’s Hospital + Health Centre and Women Against Violence Against Women, 2017; Options for Sexual Health, n.d.).
A pregnancy test completed at a doctor’s office or clinic will be covered by the Medical Services Plan (Options for Sexual Health, 2023).
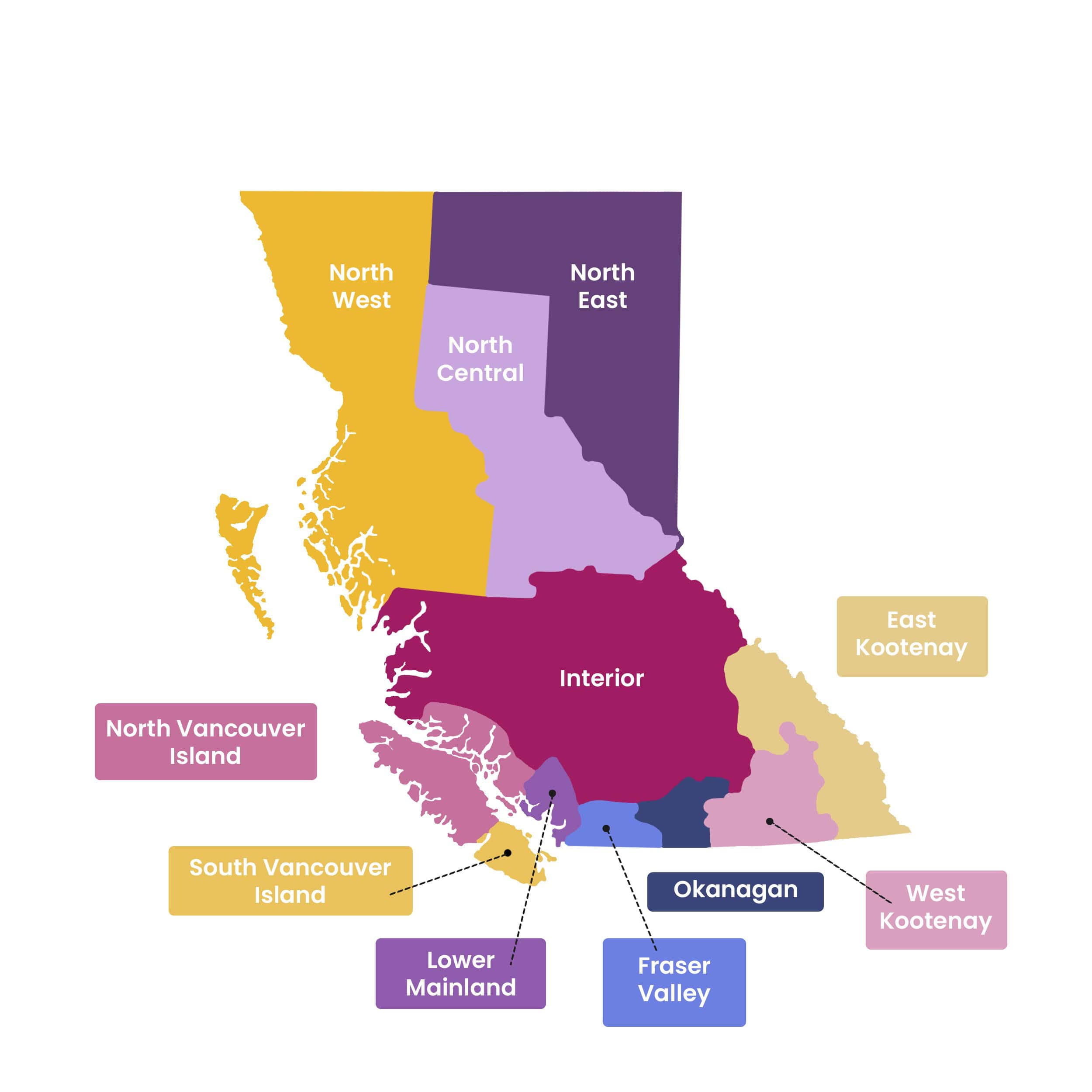
Go to the BC Centre for Disease Control Clinic Finder to locate services that do not require Medical Services Plan coverage.
Contact the Pregnancy Options Service for confidential counselling and resources at 1-888-875-3163/604-875-3163, Monday to Friday 7:30 am to 4:00 pm, or pos@cw.bc.ca.
Sex Sense and Options for Sexual Health are also resources for information, counselling, and pregnancy support.
Emergency Contraception
Emergency Contraception can be used after a sexual assault to reduce the chance of pregnancy. The “morning after pill” and the copper intrauterine device (IUD) are the two main types of emergency contraception.
Abortion
Abortion is the active termination or ending of a pregnancy through a medical procedure (Options for Sexual Health, n.d.).
Medical abortion (also known as medication abortion or the abortion pill) and surgical abortion are the two types of abortion available in BC.
Medical abortion pills require a prescription from a physician or nurse practitioner.
Medical abortion pills are available from pharmacies and are covered under PharmaCare for BC residents.
A surgical abortion is provided through abortion clinics, physicians and hospitals.
Surgical abortion is covered under the Medical Services Plan (MSP) for BC residents (Government of BC, 2022).
Click here for more information on abortion.
Contact the Pregnancy Options Service for confidential counselling and resources on local abortion providers at 1-888-875-3163/604-875-3163, Monday to Friday 7:30 am to 4:00 pm, or pos@cw.bc.ca.
Sex Sense has information on abortion including how to access abortion services. Options for Sexual Health also has a list of abortion resources here.
Sexually Transmitted Infections (STIs)
Most people with STIs don’t have symptoms; the only way to know if you have an STI is through testing (BC Women’s Hospital + Health Centre, 2018; Options for Sexual Health, n.d.; BC CDC, n.d.).
Human Immunodeficiency Virus (HIV)
HIV is a virus that targets the body’s immune system. It is transmitted through blood and body fluids.
Testing and preventative treatment is recommended for high risk situations i.e., multiple assailants; assailant is HIV positive or uses intravenous substances.
Preventative treatment must be started within 72 hours of the sexual assault.
Testing for HIV can occur between three weeks and three months after contact.
HIV testing options include: anonymous testing, point of care (rapid) testing, and self-testing (BC CDC, n.d.; BC Women’s Hospital + Health Centre, 2018).
Click here for more information on HIV testing and treatment.